Warning: I’m not a doctor, these suggestions are simply based on my personal experience, advice I’ve received and personal research.
I don’t know how some people get better from ME. I wish I did. But I’m pretty sure I’ve figured out you can get worse, and what you need to do to improve your mental, emotional and even physical state. Because CFS is an illness that affects the mind and body equally, I feel it should be treated as such. A lot of dealing with this condition appears to be common sense and discipline. Since there is a lack of reliable medical knowledge available, we must become experts on our own condition. The sooner you break away from traditional view that “my doctor/these meds will fix me” the better. You must accept that a holistic approach is the only way that your condition will improve. Read and talk to as many people as possible. Listen to your body and document how it reacts and where it is sensitive. Be willing to try anything, as long as it is realistic and within your means and limitations to do so. One of the best pieces of advice I received was to “Be your own doctor”. I would interpret this as being kind to yourself, treating your symptoms as far as possible and respecting your limits. Above all, have hope! Even though with ME/CFS it can often seem like you take one step forward, and two steps back, the illness is usually not progressive so it is likely that you are improving, even though it may be so gradual that it may be unnoticeable at first!
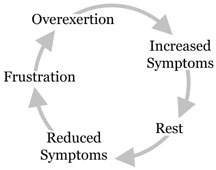
Avoid the boom & bust cycle
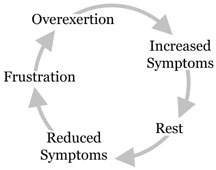
Overexertion is clearly counter-productive for those with ME/CFS. Don’t find yourself running on empty – it’s essential to rest and recharge. Stop before you are tired and do not push yourself – figure out what your limits are and stay within them. Put as much on hold as possible and delegate tasks if you can. You must learn to avoid the boom and bust cycle as this will not help your body to heal and may even cause your condition to deteriorate.
Avoid putting unnecessary strain on your immune system
If you can, I would recommend undertaking a full health check to see if there is are any underlying health issues that may be exacerbating your ME/CFS. Of course I know not all GPs will be willing, so you must be assertive or if you are able, go private. Sufferers of ME/CFS are prone to developing food or other allergies and nutritional deficiencies, which should be tested for. In my own case, I discovered I had chronic anaemia, which may have been contributing to my fatigue, so am now taking regular iron supplements. Furthermore, a fructose malabsorption was detected, a condition that was preventing my body from absorbing valuable nutrients and placing a strain on my immune system. I must now avoid sugar and fruit for the most part and have also had to address digestive disturbances caused by my IBS (irritable bowel syndrome), by logging what foods tend to upset my stomach.
In the meantime, do as much as you can to support your immune system naturally. Again, this means using common sense. Get as much fresh air and sunlight as possible, and avoid becoming chilled by making a habit of overdressing. If you are able, move to a warmer climate! If not, try regular trips to the sauna or steam room, depending on what your body can handle (the heat of the sauna is too much for me). There is no need to buy expensive products claiming to boost your immune system (which according to a study by Harvard University, may not even be scientifically viable) if you adopt a healthy diet and lifestyle. Raw fruit and vegetables and an overall healthy diet will give you essential vitamins. My doctor also recommended I take zinc, vitamin C and cod liver oil supplements. Since these are reasonably priced and widely available I decided there was no harm in boosting my nutrient intake.
With regard to diet, people with ME/CFS should cut down on sugar, white carbs and anything with “empty calories”. We need slow-burning, low GI food that gives us as much energy as possible, such as oats and whole wheat. The Food Doctor has a lot of great tips and recipes for creating a diet low in sugar and high in slow-burning foods. Drink filtered water so that your body does not have to deal with any additives in your tap water. Replace coffee and black tea with green and herbal teas. You can still get your caffeine fix from green tea. Herbal teas can also help alleviate symptoms: camomile or St John’s Wort are calming, valerian root and lavender help with sleep, ginger and lemongrass give you energy. I also drink blends of aniseed and peppermint to help with digestion and hibiscus for a sore throat. Yogi Tea and Pukka have a huge selection of teas with various health benefits.
Keep moving
To prevent your joints from seizing up and your muscles from deconditioning, it is vital for your body to remain mobile. It only takes 12 hours for your muscles to start to decondition – that fact is enough to get me off my bum! With ME/CFS, I have found it all too easy to become glued to the sofa and/or bed. However, I always feel the benefits of making an effort to go outside and even for a small walk when I didn’t feel like it. Leaving the house and getting the fresh air and sunlight on your face is also important for your mental health. Try to move your body in some way every day. Yoga and stretching are ideal anaerobic exercise that can help strengthen your muscles. If your body feels rusted up from lying around, try a short stretching session. You don’t have to attend a course, as there are plenty of yoga CDs or Youtube videos available. Look for yoga poses specifically for relaxation, stress and for strengthening the leg and arm muscles. Energizing yoga poses can help with brain fog, but remember not to push yourself. For some us, even standing up for sustained periods of time can be challenging, so slowly build up to remaining upright for 5 to 10 minutes at a time. Find an activity you can do standing, such as watching TV.
For many people with ME/CFS, pacing is a godsend, as if harnessed it can allow sufferers to regain some control of their illness. Pacing can help you take advantage of your limited energy supply by using it wisely. This includes working pre-emptive rest and scheduled rests into your day. Limiting activities (e.g. only spending 30 minutes on the computer at a time) has also proven helpful, as has switching from high-intensity tasks such as cooking to low-intensity tasks like reading. You can use a weekly or daily schedule, reminders, timers and whatever else you need to discipline yourself (get creative!) Pedometers are a great tool for pacing, as they enable you to establish a baseline, or a distance you can walk even on a bad day, and go from there. The CFIDS website has a lot of good information and tips for pacing, and offers online courses to help to implement it. Hopefully adopting some of these strategies will help your energy go further and allow you to slowly build up strength. I advise you to take baby steps and celebrate each small achievement!
Deal with any psychological issues
Over-production of adrenaline will zap your mental and physical energy, so managing psychological issues that may accompany the illness such as anxiety and depression is crucial. Try to minimize stresses in your life by staying away from people who are unsupportive and surrounding yourself with positivity as well as your loved ones. Confront situations or tasks that you have been putting off so that they are no longer weighing on you. Learning to relax (see below) is also important. Some people find writing their thoughts down in a journal to be very cathartic. Alternatively, talking about your experience with someone other than your family, such as a psychotherapist, can be very helpful. Ask your doctor about Cognitive Behavioural Therapy (CBT), which can help you deal with negative thoughts. Anti-depressants may be prescribed to you as well, which have the added benefit of helping with CFS-related sleep disturbances (particularly Amitriptyline).
Learn to relax
Anxiety and the “tired but wired” feeling, along with sleeping too much during the day make it difficult for ME/CFS sufferers to get a good night’s sleep. As mentioned above, you may need to take medication to help with your insomnia. Otherwise, adopting good sleep hygiene habits can be helpful. For instance, try to limit your naps during the day by setting an alarm. While it is evident that people with CFS need extra rest, you can learn to control when and for how long you nap. Instead of napping as a result of exertion, trying taking scheduled rests, e.g. 30 min mid-morning and another 30 min in the afternoon. Maintain regular bed- and wakeup times. Furthermore you should switch off all technology an hour before bed and trying reading instead, to calm an active mind. A gentle massage will relax your whole body, while taking a bath before bed with essential oils can also help you sleep. Aromatherapy is a fantastic tool. You can get a cheap oil burner and blend 100% essential oils such as lavender, eucalyptus and pine. I recently invested in a Soto oil diffuser, which only needs to be turned on for 20 minutes for the oil to be diffused in the room. Another great help is learning how to relax your mind using mindfulness, meditation (See my post 3 Myths About Meditation Busted) or hypnosis.
Keep a check on your emotions
It is essential to build up a support network of people who you trust who can help satisfy your emotional needs. Being chronically ill is an emotional rollercoaster, and having pillars of support will feel like a crutch during the worst times. It is also vital to educate those closest to you on your condition and be able to communicate your needs. If someone is not understanding and creating extra stress, try talking to them again. Reach out and connect with people who may be able to help, whether it be family and friends, professionals or (online) support groups. Know that it’s ok to ask for help, or ask friends to visit you if it is difficult for you to go to them. Often we are afraid to ask for support and think people will not be willing to give it. But if you try, you will be surprised. Don’t be ashamed or hide your illness either. Most people have hardships in their lives, even if they are of a different kind. Don’t be afraid to say no or miss out. Although it’s hard, remember there will always be other parties, weddings and office dos. You may be worried that cancelling on people will cause you to lose friends, but remember that the truest friends will stay with you no matter what happens in your life. Being ill, you may even cultivate new friendships in places and with people who you would never expect.
Psychotherapy or CBT can help you to accept the limits of your illness and alleviate negative emotions that stem from feeling helpless and lacking control of the situation. Focus on what you can still do rather than what you can’t, and try to focus on BEING rather than doing. Start living rather than living in wait of getting better, a mistake I have made and am now rectifying, as we do not know when or if that may happen. As humans we need to feel fulfilled, connect with others, feel loved and have a sense of purpose in our lives. You must learn to be creative within your limitations. Your condition may lead you to pick up new or forgotten hobbies that give you pleasure and suit your circumstances. Accept that this is one of the hardest things you will have to endure in your life and step up to the challenge – remember that no experience is wasted. Maintaining a positive mind-set can be easier said than done (see my post The Positivity Mandate) but it can be cultivated over time. With help, you can become emotionally self-sufficient and begin to treat yourself with empathy and compassion rather than being in a constant battle with your condition. Practice speaking to yourself in a kinder voice, for example telling yourself “It’s ok to be sick.” Try to maintain a realistic perspective too, by remembering that there are always in a worse position than yourself. If you are physically able, volunteering with the aged, severely disabled or homeless people could help you practice kindness and change your outlook.
Our lives may feel a lot smaller as a result of our condition. But ennui and a quiet life can have its blessings. You may learn to appreciate and notice the smaller things in life such as the changing seasons, a bird’s song, a child laughing… It may sound corny but I have begun to find joy in my surroundings instead of wishing I was elsewhere. To help cultivate gratitude for what we still have in our lives, I recommend keeping a gratitude journal, in which you write 5 things per day for which you are grateful. I guarantee that this practice will open your eyes to the abundance in your life.
Personally, I also find inspiration from quotes so I have a collection of the best ones pasted on my wall.
Take advantage of any treatment available to you
The NHS has 13 ME/CFS treatment clinics, offering CBT, occupational therapy and Graded Exercise Therapy. You can find more information about ME services in your area on the ME Association website.
Here is some information on treatments recommended by the NHS.
Good luck!!